Testosterone is a key component in the bodybuilding industry. This hormone is a powerful tool for anyone serious about achieving their fitness goals since it encourages muscle development, strength, and recovery. Particularly in the bodybuilding community, testosterone enanthate, and testosterone cypionate are two of the most often used testosterone esters.
But how can you pick the one that best fits your goals? This page goes into great detail on the benefits, differences, similarities, and appropriate use of testosterone enanthate and cypionate.
Whether you’re just starting your testosterone cycle or want to change things up, you’ll discover all the information you need to choose the optimal ester for your bodybuilding plan.
What Are Cypionate and Testosterone Enanthate?
Testosterone Enanthate
Testosterone enanthate is one slow-acting ester of testosterone. It is well-liked in both medical and bodybuilding contexts due to its long half-life and capacity to maintain stable testosterone levels. It is typically administered once every five to seven days by intramuscular injection.
This ester delivers testosterone into the circulation gradually, making it a fantastic choice for anyone looking for long-lasting anabolic benefits.
Testosterone Cypionate
Testosterone cypionate is another long-acting ester that is structurally identical to testosterone enanthate. It is often preferred by bodybuilders in the United States due to its accessibility and somewhat longer half-life. Similar to enanthate, it is injected intramuscularly and aids in sustaining constant testosterone levels during the cycle.
Both esters are particularly helpful for boosting muscle development, endurance, and recuperation after exercise. Subtle distinctions between the two, however, may affect your decision.
Important Similarities Between Cypionate and Testosterone Enanthate
| Testosterone Enanthate | Testosterone Cypionate | |
|---|---|---|
| Chemical Structure | It has a 7-carbon ester chain | It has an 8-carbon ester chain |
| Release Time | Slower release into the bloodstream (4-5 days half-life) | Slightly slower release compared to Enanthate (5-7 days half-life) |
| Administration Frequency | Typically once a week or every two weeks | Usually once a week to maintain stable testosterone levels |
| Popular Usage | Common in Europe and outside of the United States | Predominantly used in the United States |
Before exploring the differences between these two supplements, it is important to acknowledge the many similarities between them.
- Goal: Both are used for testosterone replacement treatment (TRT) and bodybuilding to provide anabolic effects. By raising or restoring testosterone levels, they promote muscle development, recovery, and overall performance improvement.
- The ratio of anabolic to androgenic: Both esters have the same anabolic to androgenic ratio (100/100). This indicates that they have the same potent performance impacts on strength and muscle growth.
- Administration: Because both are administered intramuscularly and provide a gradual release of hormones, fewer injections are required throughout the cycle.
- Benefits of Performance:
- Encourages the building of lean muscle mass
- Boosts strength and power
- Quickens recovery in between workouts
- Assists in the reduction of body fat when combined with a healthy diet.
- Side Effects: Both have the potential to cause gynecomastia, acne, elevated blood pressure, and water retention. These dangers can be reduced with the use of appropriate post-cycle treatment (PCT).
However, even little variations can have a significant impact on overall experience and performance.
Important Distinctions Between Cypionate and Enanthate

1. The Half-Life and Injection Frequency
For testosterone enanthate, the half-life is around four to five days. To maintain optimal levels, bodybuilders often take testosterone once every five to seven days.
Users can inject testosterone cypionate less frequently, typically once every seven days, because of its somewhat longer half-life of five to six days.
In conclusion, if you value injection frequency, testosterone cypionate may be more sensible. However, since the difference is small, personal choice plays a role here.
2. Availability
Testosterone enanthate is widely available internationally and is used more often overseas. Often, it is slightly less costly than Cypionate.
Although testosterone cypionate is more often used in the US, it may be harder to find in other countries.
Takeaway: Choose the ester that is more readily available in your location to avoid unnecessary expenses or supply issues.
3. Carrier Oil
According to some users, Cypionate has a thicker viscosity, which, depending on the carrier oil used, could irritate the injection site more.
Enanthate often receives fewer complaints.
Conclusion: If one ester makes you uncomfortable, you might want to try the other one to see if it makes things better.
Which Is More Effective in Bodybuilding?
Selection is often dependent on personal experience, even though the anabolic effects of the two esters are almost identical. For instance, bodybuilders used to weekly injections could find it easier to keep up a Testosterone Cypionate cycle, while those who want more exact control over their fluctuations would choose Enanthate.
In conclusion, both testosterone enanthate and testosterone cyclopamine are excellent for bodybuilding. Your goals, preferences, and the chemicals’ accessibility should all play a role in your choice.
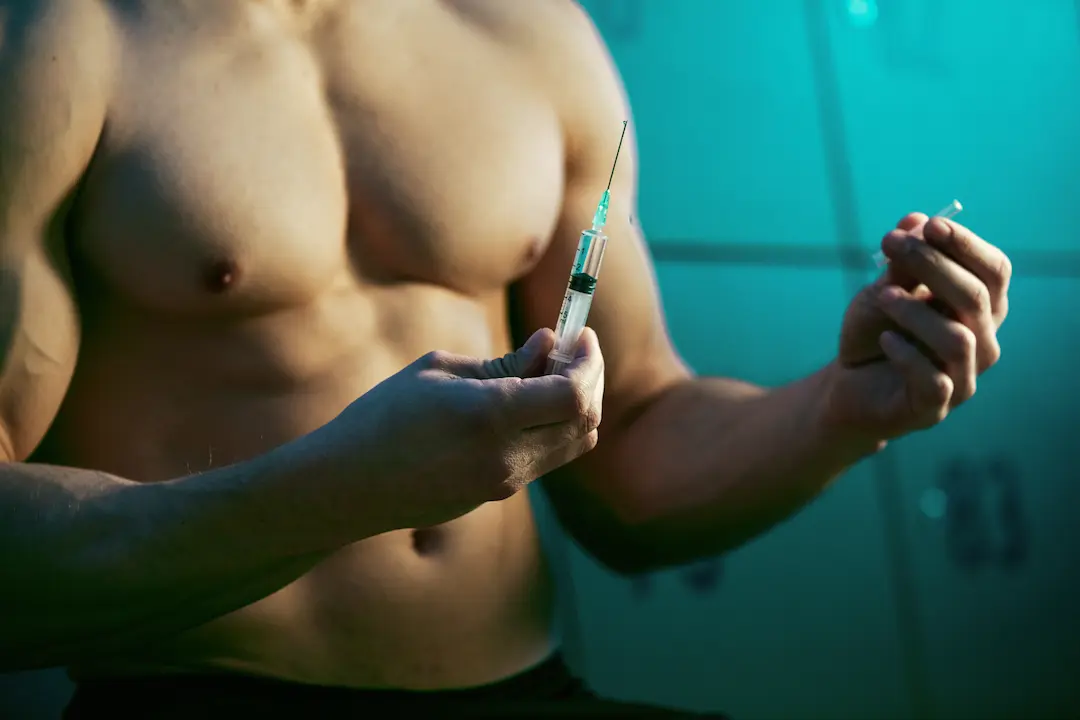
How to Safely Use Cypionate or Testosterone Enanthate

Safety should always come first when using testosterone of any kind for bodybuilding. Planning is essential for both enanthate and cypionate in order to maximize benefits and minimize negative effects.
Suggested Doses

Start with dosages that are easy for beginners. Depending on your degree of experience, the following is a general guide to follow:
Novice Users: 250-500 mg weekly
Intermediate Users: 500-750 mg weekly
Expert Users: 750-1000 mg weekly
Duration of Cycle
Both esters typically have a cycle length of 8-12 weeks. This length of time gives you enough time to notice improvements without putting too much strain on your body.
Incorporate with PCT (Post Cycle Therapy)
After a testosterone cycle ends, use PCT to resume your body’s natural hormone production. Clomid or Nolvadex are common choices for four to six weeks following a cycle.
Always Get Expert Guidance
Before starting any cycle, see a healthcare provider or fitness expert to create a plan specific to your goals and present state of health. Remember that our Steroiduck team mate Dr. Grant F is always ready to help and answer every of Your question ragarding Testosterone Cypionate or Enanthate
Concluding Remarks on Selecting Cypionate or Enanthate
Both testosterone enanthate and cypionate are excellent choices for bodybuilders looking to enhance their performance and physique. Since these esters have almost identical benefits and effects, the optimum choice often depends on availability, injection frequency, and individual preference.
Regardless of the ester you choose, prioritize safety, follow a structured cycle, and be consistent with your workout and nutrition.
Are you wondering how to get the most out of your bodybuilding workouts? Sign up for our newsletter to have expert guidance on nutrition, supplements, and fitness sent directly to your inbox!
