Testosterone Replacement Therapy (TRT): Evidence-Based Treatment Options for Low T Symptoms

Millions of men worldwide experience declining testosterone levels as they age, leading many to consider testosterone replacement therapy as a potential solution. Testosterone replacement therapy (TRT) is a medical treatment that helps restore testosterone levels to a normal range in men diagnosed with clinically low testosterone, potentially improving symptoms like fatigue, reduced muscle mass, and decreased libido.
We’ll explore how TRT works and help you understand whether this treatment might be right for your situation. The therapy involves various methods of delivering testosterone to the body, but it’s not a decision to take lightly.
Throughout this guide, we’ll examine the science behind testosterone’s role in men’s health, discuss the potential benefits and risks you should know about, and cover the different treatment options available. We’ll also address common concerns about monitoring requirements during TRT and lifestyle factors that can impact your treatment success.
What Is Testosterone Replacement Therapy (TRT)?
Testosterone replacement therapy involves medical treatment to restore normal testosterone levels in men with testosterone deficiency. This therapy addresses male hypogonadism through various treatment methods and has evolved significantly since its introduction in medical practice.
Definition and Purpose
Testosterone replacement therapy is a medical treatment that restores testosterone levels in men who have low testosterone. TRT has been used in millions of men worldwide to treat diminished libido and erectile dysfunction, and to improve strength and physical function.
The primary purpose of testosterone therapy is to treat male hypogonadism. This condition occurs when the body does not produce enough testosterone naturally.
Common symptoms TRT addresses include:
- Low sex drive
- Erectile dysfunction
- Fatigue and low energy
- Muscle weakness
- Mood changes
We use TRT to bring testosterone levels back to normal ranges. This helps restore proper body functions that depend on adequate testosterone levels.
History and Evolution of TRT
Testosterone therapy began in the 1930s when scientists first isolated testosterone. Early treatments used animal-derived hormones with limited success.
The 1940s brought synthetic testosterone development. This marked a major step forward in treating testosterone deficiency effectively.
Modern TRT offers multiple delivery methods. These include gels, patches, testosterone injections, and implants that provide more consistent hormone levels.
Recent FDA examinations of TRT data have shaped current treatment guidelines. This has led to stricter requirements for diagnosis and monitoring.
Today’s testosterone replacement therapy focuses on personalized treatment plans. We now better understand proper dosing and monitoring requirements for safe treatment.
Who Needs TRT?
Men with clinically diagnosed testosterone deficiency are candidates for TRT. This requires both low testosterone blood tests and symptoms of hypogonadism.
Primary hypogonadism occurs when testicles cannot produce enough testosterone. Secondary hypogonadism happens when the brain does not signal testosterone production properly.
Age-related testosterone decline affects many older men. However, normal aging alone does not automatically qualify someone for testosterone therapy.
Medical conditions that may lead to TRT need include:
- Genetic disorders affecting hormone production
- Injury to testicles or pituitary gland
- Cancer treatments
- Chronic diseases affecting hormone levels
We must confirm both low testosterone levels and related symptoms before starting treatment. Healthcare providers should discuss with patients the potential benefits and risks of TRT before beginning therapy.
Young men with testosterone deficiency may need lifelong treatment. Older men require careful evaluation to determine if benefits outweigh potential risks.
Understanding Testosterone and Its Role
Testosterone serves as the primary male hormone that controls everything from muscle development to sexual function. We see how testosterone production naturally changes with age and how various factors can impact these crucial hormone levels.
Testosterone Production in the Body
Our bodies produce testosterone through a complex system involving the brain and testicles. The hypothalamus in the brain releases a hormone that signals the pituitary gland. This gland then sends luteinizing hormone to the testicles.
The testicles respond by making testosterone in special cells called Leydig cells. Most testosterone production happens during sleep. We typically see the highest levels in the morning.
Normal testosterone levels range from 300 to 1,000 nanograms per deciliter in adult men. These levels naturally decline by about 1-2% each year after age 30. Some men experience faster drops than others.
The body also converts some testosterone into other hormones like estrogen and DHT. This conversion happens in various tissues throughout our bodies.
Functions in Male Health
Testosterone controls many important functions in men’s health. Sexual function and libido depend heavily on adequate testosterone levels. Low levels often lead to reduced sex drive and problems with erections.
We see testosterone’s impact on physical development too. It builds muscle mass and muscle strength while affecting how our bodies store fat. Men with normal levels typically have less belly fat.
Bone density relies on testosterone to stay strong throughout life. Low levels increase the risk of fractures and osteoporosis as we age.
Testosterone also affects sperm production in the testicles. Understanding testosterone replacement therapy shows that low levels can reduce fertility.
Mental health connects to testosterone too. Normal levels support mood stability and energy. Low testosterone often causes fatigue and depression.
Factors Affecting Testosterone Levels
Several factors influence our testosterone levels throughout life. Age remains the biggest factor for most men. Aging men naturally produce less testosterone over time.
Health conditions can lower testosterone significantly:
- Obesity reduces production
- Diabetes affects hormone balance
- Sleep disorders disrupt nighttime production
- Chronic stress elevates cortisol, which blocks testosterone
Lifestyle choices also matter. Regular exercise, especially weight lifting, helps maintain healthy levels. Good sleep habits support natural production cycles.
Medications can interfere with testosterone. Opioid pain medications and some antidepressants commonly cause reductions. We also see drops from excessive alcohol use and smoking.
Injury to the testicles or certain genetic conditions can affect production from birth. These cases often require medical evaluation and treatment.
Symptoms and Diagnosis of Low Testosterone
Low testosterone affects men differently, but certain physical and emotional symptoms consistently appear when testosterone levels drop below normal ranges. Proper diagnosis requires both clinical symptoms and laboratory testing to confirm testosterone deficiency.
Recognizing Symptoms of Low Testosterone
Physical symptoms of low testosterone often develop gradually over months or years. Men frequently experience erectile dysfunction, reduced muscle mass, and increased body fat around the waist.
Low libido ranks among the most common early signs. Many men notice decreased interest in sexual activity before other symptoms appear.
Energy-related symptoms include persistent fatigue, reduced stamina, and difficulty concentrating. Sleep problems and irritability also commonly occur with testosterone deficiency.
Depression can develop alongside low testosterone levels. Men may experience mood swings, anxiety, or feelings of sadness that seem unexplained.
Body composition changes become visible over time. We see decreased muscle strength, increased belly fat, and sometimes enlarged breast tissue in men with low T.
Hair loss, particularly body and facial hair thinning, may accompany other symptoms. Hot flashes, similar to those in menopause, affect some men with severely low testosterone.
Diagnostic Criteria and Testing
Blood tests measure total testosterone levels in the morning when levels peak naturally. Normal ranges typically fall between 300-1000 ng/dL, though symptoms with total T levels below specific thresholds help guide diagnosis.
Free testosterone testing provides additional information since this represents the active hormone available to tissues. Some men have normal total testosterone but low free testosterone.
We recommend testing on at least two separate mornings before 10 AM. Testosterone levels fluctuate throughout the day and can vary between testing sessions.
Diagnosis requires both low testosterone levels and related clinical symptoms rather than laboratory results alone. Men without symptoms typically don’t need treatment despite borderline low levels.
Additional blood work may include luteinizing hormone (LH), follicle-stimulating hormone (FSH), and prolactin levels. These help determine whether the problem originates in the testicles or brain.
Differentiating Causes of Low T
Primary hypogonadism occurs when testicles don’t produce enough testosterone despite normal brain signals. Causes include injury, infection, chemotherapy, or genetic conditions.
Secondary hypogonadism results from problems with the hypothalamus or pituitary gland. These brain areas control testosterone production through hormone signals.
Medical conditions frequently contribute to low testosterone. Obesity, diabetes, sleep apnea, and chronic liver or kidney disease can all reduce testosterone levels.
Certain medications lower testosterone production. Opioid pain medications, steroids, and some antidepressants commonly affect hormone levels.
Age-related decline represents the most common cause. Testosterone drops approximately 1% per year after age 30, though not all men develop symptoms requiring treatment.
Stress, poor sleep, and excessive alcohol consumption can temporarily suppress testosterone production. Addressing these lifestyle factors sometimes improves levels without medical intervention.
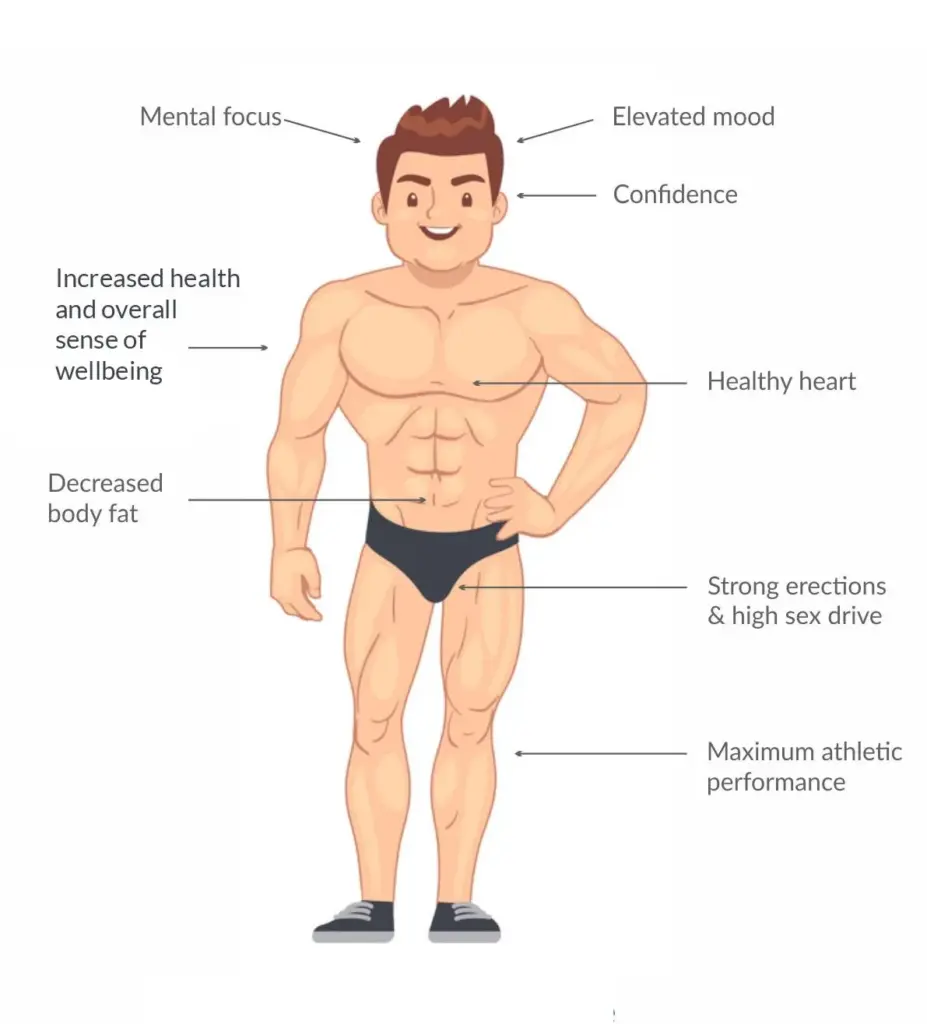
Benefits of Testosterone Replacement Therapy

Testosterone replacement therapy offers significant improvements across physical health, sexual function, and mental well-being. These benefits help men restore normal hormone levels and improve quality of life.
Physical Benefits
Muscle Mass and Strength
We see notable increases in muscle mass when men start testosterone therapy. The hormone helps build lean muscle tissue more effectively than diet and exercise alone.
Muscle strength improves within the first few months of treatment. Men report being able to lift heavier weights and perform daily activities with less effort.
Bone Health
Bone density increases with testosterone replacement. This is especially important for older men who face higher risks of fractures.
The therapy helps prevent bone loss that naturally occurs with aging. Stronger bones reduce the chance of breaks from falls or accidents.
Body Composition Changes
| Change | Timeframe | Effect |
|---|---|---|
| Fat reduction | 3-6 months | Less belly fat |
| Muscle gain | 2-4 months | Increased lean mass |
| Energy levels | 2-8 weeks | More stamina |
Sexual Health Improvements
Enhanced Libido
Research shows strong evidence for TRT benefits on sexual desire. Men experience increased interest in sexual activity within weeks of starting treatment.
Sex drive often returns to levels similar to younger years. This improvement happens gradually as testosterone levels stabilize.
Better Sexual Function
Erections become stronger and more frequent with proper testosterone levels. Many men notice improvements in both the quality and duration of erections.
Sexual performance and satisfaction increase for most patients. The combination of higher libido and better function creates positive changes in relationships.
Cognitive and Emotional Effects
Mood Improvements
We observe significant mood changes in men receiving testosterone therapy. Depression symptoms often decrease as hormone levels normalize.
Irritability and anxiety tend to reduce within the first month of treatment. Men report feeling more emotionally stable and balanced.
Mental Clarity
Concentration and focus improve with testosterone replacement. Many patients describe feeling mentally sharper and more alert.
Memory function often gets better, especially for recent events. This cognitive boost helps with work performance and daily tasks.
Energy and Motivation
Fatigue decreases as testosterone levels rise. Men find they have more energy for exercise, work, and social activities.
Motivation to pursue goals and hobbies often returns. This renewed drive helps improve overall life satisfaction and productivity.
Risks and Side Effects of TRT
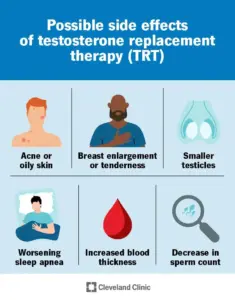
TRT carries several potential risks ranging from minor skin issues to serious cardiovascular complications. Understanding these risks helps patients make informed decisions about treatment.
Common Adverse Effects
Many men experience mild to moderate side effects when starting TRT. These effects often improve as the body adjusts to treatment.
Skin and cosmetic changes are frequent complaints. Acne breakouts occur in about 15-20% of men on TRT. The increased testosterone can stimulate oil glands, leading to pimples on the face, chest, and back.
Gynecomastia affects some men during treatment. This breast tissue enlargement happens when testosterone converts to estrogen in the body. The condition usually develops gradually over several months.
Fluid retention is another possible side effect of TRT. Men may notice swelling in their hands, feet, or ankles. Weight gain of 5-10 pounds is common in the first few months.
Sleep problems can worsen with TRT. Men with existing sleep apnea may experience more breathing interruptions at night. This happens because testosterone can affect throat muscle tone.
Hair loss may accelerate in men who are already prone to male pattern baldness. The therapy can speed up the natural hair loss process.
Serious Health Risks
TRT carries several serious health risks that require careful monitoring. These complications can be life-threatening if not detected early.
Cardiovascular risks are the most concerning. Studies show increased risk of heart attacks in men over 65 within 90 days of starting treatment. The risk appears highest in older men with existing heart problems.
Blood clots pose a significant danger. TRT increases red blood cell production, which can make blood thicker. This heightens thrombotic risks and may lead to dangerous clots in the legs or lungs.
Men face higher cardiovascular risk if their hematocrit reaches or exceeds 52% during the first year of therapy. Regular blood tests are essential to monitor these levels.
Prostate concerns require ongoing attention. TRT may worsen benign prostatic hyperplasia (BPH) in some men. This can lead to difficulty urinating and other bladder problems.
The relationship between TRT and prostate cancer remains unclear. While TRT doesn’t appear to cause prostate cancer, it may accelerate existing tumors.
Contraindications and Precautions
Certain medical conditions make TRT dangerous or inappropriate. We must carefully screen patients before starting treatment.
Absolute contraindications include active prostate cancer and breast cancer in men. TRT can fuel the growth of hormone-sensitive cancers, making these conditions extremely dangerous to treat.
Men with severe heart failure should avoid TRT. The therapy can worsen fluid retention and strain an already weakened heart.
Sleep apnea requires special consideration. Men with moderate to severe obstructive sleep apnea may experience worsening symptoms. Treatment of sleep apnea should occur before starting TRT.
Men planning to father children should know that TRT causes infertility. The therapy shuts down natural testosterone production and sperm formation.
High hematocrit levels above 50% require treatment delays. Men with naturally thick blood face increased clot risks with TRT.
Liver disease can worsen with certain forms of testosterone. Oral testosterone preparations carry the highest risk of liver damage.
Methods and Forms of Testosterone Replacement Therapy
Doctors can deliver testosterone treatment through several proven methods, each with unique benefits and considerations. The main approaches include injections, skin applications, and specialized delivery systems that help maintain steady hormone levels.
Injectable Testosterone
Injectable forms represent the oldest form of testosterone replacement therapy available to patients. We typically administer these shots into muscle tissue every 1-4 weeks depending on the specific formulation.
Common Injectable Types:
- Testosterone cypionate (weekly or bi-weekly)
- Testosterone enanthate (weekly or bi-weekly)
- Testosterone undecanoate (every 10-12 weeks)
Injectable testosterone often produces the most significant increases in blood levels. However, patients may experience fluctuations between doses, with levels peaking shortly after injection and declining before the next dose.
Many men prefer injections because they require less frequent dosing compared to daily applications. The main drawbacks include potential injection site soreness and the need for regular medical visits or self-administration training.
Transdermal Applications
Transdermal testosterone treatment delivers hormones through the skin using gels, patches, or creams. These methods provide more stable blood levels throughout the day compared to injections.
Available Forms:
- Gels: Applied daily to shoulders, arms, or abdomen
- Patches: Worn on skin for 24 hours before replacement
- Creams: Rubbed into skin once or twice daily
Gel concentrations include 1% forms as unit dose packets of 25 mg/2.5 g or 50 mg/5 g. These applications absorb through the skin over several hours.
Transdermal options work well for men who want to avoid injections. The main concerns include skin irritation and the risk of transferring testosterone to family members through skin contact.
We recommend washing hands thoroughly after application and covering treated areas with clothing.
Other Delivery Methods
Several alternative delivery methods offer unique advantages for specific patient needs. These specialized forms can address concerns about daily applications or injection schedules.
Nasal Gels: Applied inside the nostrils 2-3 times daily. This method avoids skin transfer risks but requires multiple daily doses.
Pellet Implants: Small pellets inserted under the skin every 3-6 months. These provide steady hormone release but require minor surgical procedures for placement and removal.
Oral Tablets: Newer formulations that avoid liver problems associated with older oral testosterone. These are taken twice daily with meals.
Buccal Tablets: Placed against the gum and dissolve over 12 hours. Patients use these twice daily for consistent hormone delivery.
Each alternative method serves patients with specific preferences or medical considerations that make standard injections or gels less suitable for their testosterone treatment plan.
Monitoring, Management, and Lifestyle Considerations
Regular monitoring helps detect potential side effects early while lifestyle changes can enhance treatment benefits. Proper management addresses fertility concerns and long-term health risks in aging men.
Monitoring Testosterone Levels
We recommend checking testosterone levels 3-6 months after starting TRT. Blood tests should happen in the morning when testosterone is naturally highest.
Key monitoring schedule:
- Baseline levels before treatment
- 3-month follow-up after starting
- Every 6-12 months during stable treatment
Healthcare providers track both total and free testosterone. Total testosterone measures all testosterone in blood. Free testosterone shows the active hormone available to tissues.
Improving monitoring rates helps optimize treatment and reduce risks. Many patients don’t get proper follow-up care.
We also monitor red blood cell counts and liver function. These tests catch problems before they become serious.
Managing Side Effects
Common side effects include increased red blood cell production and fluid retention. Some men experience mood changes or sleep problems.
Potential side effects to watch:
- High red blood cell count
- Swelling in legs or ankles
- Skin reactions at injection sites
- Mood swings or irritability
Managing adverse effects requires understanding possible complications. Healthcare providers adjust doses or change delivery methods when problems occur.
We address decreased bone density concerns in aging men. TRT can help strengthen bones when testosterone is low.
Obesity may worsen some side effects. Weight management becomes important during treatment.
Impact on Fertility and Long-Term Health
TRT significantly affects male fertility by reducing sperm production. The treatment signals the body to stop making its own testosterone.
Testosterone replacement suppresses spermatogenesis in most men. Sperm counts often drop to very low levels within months.
Young men who want children should consider fertility preservation. We discuss sperm banking before starting treatment.
Fertility considerations:
- Sperm production usually decreases within 2-3 months
- Recovery may take 6-18 months after stopping TRT
- Some men don’t fully recover normal sperm counts
Long-term cardiovascular effects remain under study. We monitor heart health regularly during treatment.
Lifestyle Modifications
Exercise and diet changes can boost TRT effectiveness. Regular strength training helps build muscle mass and bone density.
Recommended lifestyle changes:
- Strength training: 2-3 sessions per week
- Cardiovascular exercise: 150 minutes weekly
- Healthy diet: Focus on protein and whole foods
- Weight management: Maintain healthy BMI
Lifestyle interventions work well with testosterone treatment for better results. Combined approaches often work better than TRT alone.
Sleep quality affects testosterone production. We recommend 7-9 hours of sleep nightly.
Stress management helps maintain hormonal balance. Chronic stress can interfere with treatment effectiveness.
Limiting alcohol and avoiding smoking support better treatment outcomes. These habits can lower natural testosterone production in aging men.
Frequently Asked Questions
What potential side effects should one be aware of when considering testosterone replacement therapy?
Sleep apnea may worsen in some men taking testosterone therapy. Fluid retention can occur, leading to swelling in the legs or ankles.
Skin reactions like acne or oily skin affect many users. Some men experience mood changes, including increased irritability or aggression.
Prostate enlargement may happen, which can make urination difficult. Breast enlargement or tenderness can also develop in some cases.
How does the cost of testosterone replacement therapy vary based on treatment methods?
Insurance coverage varies widely between providers and specific treatments. Many plans require prior authorization before covering testosterone therapy.
Cash-based clinics and online services often charge different rates than traditional medical practices. Generic testosterone preparations usually cost less than brand-name versions.
Monthly expenses can range from under $50 for injections to several hundred dollars for newer delivery methods. Lab monitoring adds extra costs throughout treatment.
What criteria must be met to be a candidate for testosterone replacement therapy?
Age typically plays a role, as testosterone naturally declines with aging. Medical history screening helps identify men who might face higher risks.
Prostate cancer must be ruled out before starting therapy. Heart disease history requires careful evaluation due to potential cardiovascular risks.
Other hormone levels may need testing to ensure testosterone deficiency is the primary issue. Some conditions like sleep apnea may need treatment first.
Can testosterone replacement therapy be discontinued abruptly, and if so, what are the implications?
Withdrawal symptoms can include fatigue, depression, and loss of muscle mass. Sexual function often declines rapidly when treatment ends abruptly.
Gradual tapering may help reduce withdrawal effects in some cases. Medical monitoring helps track hormone recovery and manage symptoms.
Natural testosterone production may never fully return to pre-treatment levels. Some men require ongoing hormone support even after attempting to stop.
What changes should one expect to see after initiating testosterone replacement therapy?
Muscle mass and strength gains become noticeable after several months of consistent treatment. Fat loss may occur gradually, particularly around the midsection.
Sleep quality often improves within the first month of therapy. Mental clarity and focus may enhance as testosterone levels normalize.
Body hair growth and voice changes are less common in adult men. Red blood cell production increases, which requires regular monitoring through blood tests.
Are there different types of testosterone replacement options, and how do they compare?
Topical gels and creams absorb through skin daily. These offer steady hormone delivery but can transfer to others through skin contact.
Patches stick to skin and release testosterone over 24 hours. They provide consistent levels but may cause skin irritation in some users.
Pellets implanted under the skin last three to six months. This method requires minor surgical procedures but eliminates daily applications.
Nasal gels offer convenient application but require multiple daily doses. Each delivery method has different patient satisfaction rates based on convenience and effectiveness.
