Steroid injections are medical treatments used to alleviate inflammation and reduce pain in a variety of conditions such as arthritis, bursitis, and tendinitis. While they can be highly effective, it’s crucial to adhere to proper safety protocols to minimize risks and complications. Healthcare providers must be well-versed in the indications for steroid use, the potential side effects, and the techniques for administration to ensure patient safety and optimal therapeutic outcomes.
When it comes to steroid injections, pre-injection considerations are as important as the technique itself. Providers should assess the patient’s medical history, current medications, and potential allergy to components in the injection. Sterile technique is imperative to prevent infection, and precise anatomical knowledge is required to place the medication effectively. After the procedure, following evidence-based post-injection protocols helps in monitoring for side effects and ensures that the patient receives comprehensive care.
Quick Summary
- Safe steroid injection practices require knowledge of proper technique and potential side effects.
- Prior to injection, thorough patient evaluation and adherence to sterile protocols are essential.
- Post-injection care involves monitoring for complications and managing patient recovery effectively.
Understanding Steroid Injections
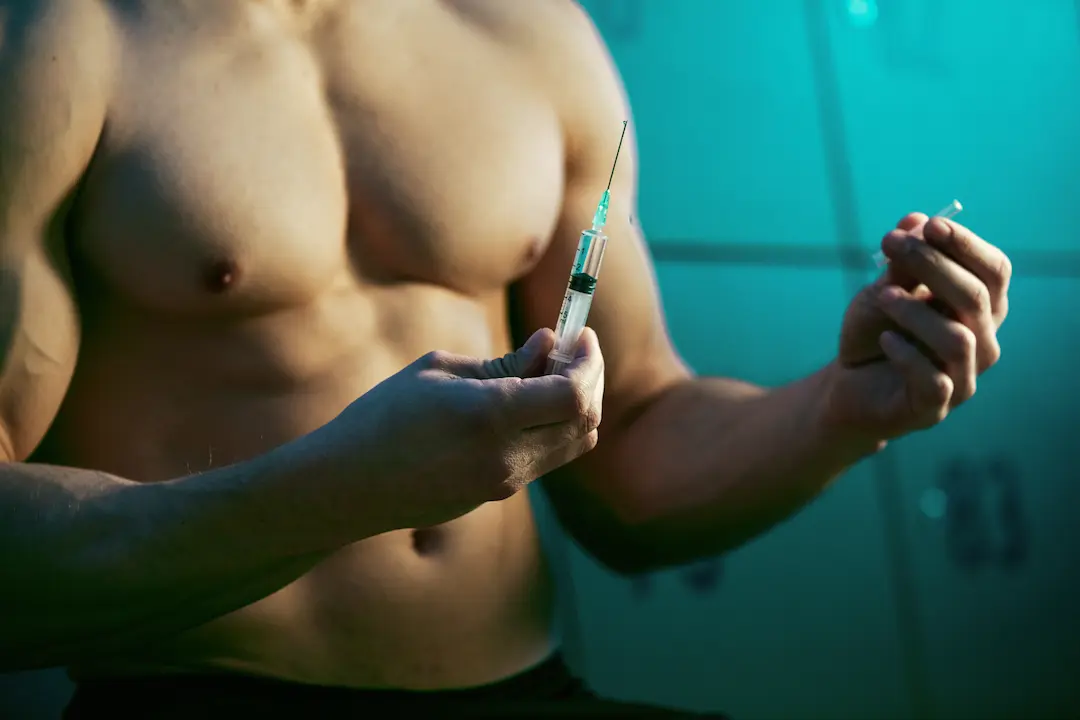
Steroid injections are medical treatments that deliver corticosteroids directly into an area of the body to reduce inflammation and alleviate pain. These injections are used to treat a variety of conditions and are not to be confused with anabolic steroids used for bodybuilding.
Types of Steroid Injections
There are several key types of steroid injections, each designed for specific applications:
- Cortisone Shots: Typically administered to ease pain and swelling in joints.
- Triamcinolone: Often used for skin conditions and allergic reactions.
- Betamethasone: Commonly for more severe inflammatory issues.
- Prednisolone and Hydrocortisone: These can serve as systemic treatments for widespread inflammation.
Glucocorticoids are the most common type of corticosteroid used in steroid injections. They mimic cortisol, a hormone naturally produced by the adrenal glands.
Mechanism of Action
Corticosteroids function by mimicking hormones that naturally occur in the body. Specifically, they resemble cortisol, which is produced by the adrenal cortex. Cortisol plays a crucial role in reducing inflammation in the body, and corticosteroids amplify this effect. They work by downregulating the production of substances that trigger inflammatory and immune responses, effectively reducing tissue damage from inflammation.
For example, when cortisone—a synthetic glucocorticoid—is injected, it can help to rapidly decrease inflammation, leading to pain relief and improved function of the affected area.
The specificity of the steroid’s effect largely depends on the precise nature of the tissue into which it is injected, which in turn influences its therapeutic outcomes.
References
Pre-injection Safety Considerations

Before administering a steroid injection, healthcare providers must ensure patient safety through comprehensive patient assessment and awareness of any contraindications and precautions.
Patient Assessment
Healthcare providers must conduct a thorough patient assessment prior to administering a steroid injection. This includes obtaining a detailed medical history and performing a physical examination. Patient history should encompass any known allergies, especially to medications or components found in the injectable steroid solution. It is also critical to review the patient’s current list of medications with a focus on blood thinners, which can increase the risk of bleeding. Providers should monitor patients with diabetes as corticosteroids can elevate blood sugar levels. Additionally, a thorough assessment of liver, heart, and immune system function is necessary due to the potential for systemic effects after the injection.
- Medical History: Evaluate for allergies, current medications, and status of chronic conditions.
- Physical Examination: Focus on the intended injection site and surrounding areas.
Contraindications and Precautions
Certain conditions may serve as contraindications or require precautions when considering steroid injections. Patients with uncontrolled conditions such as high blood pressure or infections should not receive injections until these issues are adequately managed. Corticosteroids can weaken the immune system, hence it is prudent to avoid injections in patients with systemic infections or those who are immunocompromised. Additional precautions should be taken for patients with compromised liver function, as the metabolism of steroids can be altered, increasing the potential for adverse effects.
- Contraindications: Include uncontrolled blood pressure, systemic infections, and poor immune function.
- Precautions: Take extra care with patients who have liver issues, diabetes, or are on blood thinners.
How to Inject Steroids – Injection Techniques

Accurate and safe steroid injections require precise technique, involving careful needle selection, stringent site preparation, and following defined injection procedures.
Needle Selection
Choosing the right needle is critical for any injection. The length and gauge of a needle depend on the injection site and the depth of tissue it must penetrate. For intramuscular injections, typically a 22 to 25 gauge needle is used, with length varying from 1 to 1.5 inches for adults. For joints, a larger gauge may be necessary to administer a local anesthetic or steroids.
- Muscles and Joints: Use a 22 to 25 gauge, 1 to 1.5-inch needle
- Veins: Generally smaller gauges like 25 to 27
Site Preparation
Site preparation involves using an aseptic technique to avoid infection. The targeted area must be thoroughly cleaned with an antiseptic solution. If ultrasound is used to locate the injection site, ensure the settings are adjusted correctly to visualize the target area.
- Clean the injection site thoroughly with an antiseptic solution.
- If using ultrasound, optimize settings to clearly view the injection area.
Injection Procedures
Proper injection technique is essential for the safety and efficacy of the treatment. For intramuscular injections, the needle should be inserted at a 90-degree angle to the skin. Aspirate before injecting to ensure the needle is not in a vein. Perform the procedure in settings equipped to handle potential complications.
Intramuscular Injection:
- Insert needle at 90 degrees to the skin’s surface.
- Aspirate before injecting to avoid veins.
Local Anesthetic:
- Administered prior to steroid to reduce pain.
Post-Injection Protocols

After a steroid injection, proper aftercare is critical for reducing the risk of unwanted side effects and promoting recovery. It involves managing immediate reactions post-injection and careful monitoring during the aftercare period.
Managing Immediate Reactions
Immediate Aftercare:
- Apply ice to the injection site to alleviate swelling and redness.
- Avoid applying heat or pressure to the injected area, which can exacerbate swelling.
Aftercare and Monitoring
- Monitoring for Side Effects: Patients should observe for signs of increased redness, swelling, or bruising, which might indicate an infection or other complications.
- Pain Relief: For effective pain relief, over-the-counter medications such as acetaminophen can be used; however, avoid NSAIDs like ibuprofen which could increase bleeding.
- Activity Level: Patients should limit strenuous activities for several days to allow the injected area to heal.
Potential Complications and Management

This section elaborates on the recognition of adverse events following steroid injections and the strategies for medical intervention to manage these complications.
Recognizing Adverse Events
Post-steroid injection complications can vary but it’s crucial for both patients and healthcare providers to be vigilant. Risk factors for complications can be patient-specific or related to the injection technique. Side effects may include pain at the site of injection, inflammation, and elevation in blood sugar levels. More serious complications, although rare, can include infection or joint infection, nerve damage, and the formation of abscesses.
- Symptoms to watch for include:
- Excessive swelling or redness
- Persistent pain or discomfort
- Fever or chills
- Changes in skin color or sensation around the injection site
Intervention Strategies
Early identification and management of adverse events are the cornerstones of reducing harm and ensuring patient relief. If an infection is suspected, culture tests and prompt antibiotic therapy may be necessary. Elevated blood sugar levels should be monitored and managed according to existing diabetic protocols. For abscesses or severe inflammation, individuals may require surgical intervention or additional medical treatment.
- Community health strategies include:
- Educating patients about the symptoms of complications
- Ensuring sterile techniques to reduce the risk of infection
- Close monitoring of patients with diabetes for changes in blood sugar
The goal is to balance the therapeutic benefits of steroid injections with precautionary measures to ensure patient safety and the minimization of potential complications.
References
- American Academy of Orthopaedic Surgeons. (n.d.). Corticosteroid Injections. AAOS. https://orthoinfo.aaos.org/en/treatment/corticosteroid-injections
Frequently Asked Questions

These questions cover critical information on the safety, techniques, and aftercare considerations regarding steroid injections.
What are the best techniques for avoiding veins during steroid injections?
Professionals typically employ techniques such as aspiration, which involves pulling back on the syringe before injecting to ensure the needle is not in a vein. They also use anatomical knowledge to select a site that minimizes the risk of intravascular injection.
How does a steroid injection affect the immune system, and for how long?
A steroid injection can suppress the immune system by diminishing the body’s inflammatory response. The duration of this effect varies but can last for a few weeks to a few months depending on the dose and type of steroid used.
What are the different types of steroid injections commonly used?
There are several types of steroid injections, including cortisone, prednisolone, and methylprednisolone. These are often used to reduce inflammation in conditions like arthritis, tendinitis, and bursitis.
What should one consider when preparing for a steroid injection?
Before receiving a steroid injection, individuals should discuss their current medications, allergies, and medical history with their healthcare provider to prevent adverse effects. It’s also important to follow any fasting instructions if the steroid is to be administered via the intravenous route.
What are the potential side effects and disadvantages of cortisone injections?
Possible side effects of cortisone injections include joint infection, nerve damage, thinning of nearby bone, tendon rupture, and elevated blood sugar levels in diabetics. Individuals may also experience “steroid flare,” temporary pain and inflammation in the injection area.
How should one care for the injection site after receiving a cortisone shot?
Post-injection care involves keeping the area clean, avoiding strenuous activities for several days, and applying ice if there is pain. It’s crucial to monitor the site for signs of infection or significant reactions and contact a healthcare provider if any concerning symptoms arise.
References
- American Academy of Orthopaedic Surgeons. (n.d.). Corticosteroid Injections. OrthoInfo. https://orthoinfo.aaos.org/en/treatment/corticosteroid-injections/
- Cleveland Clinic. (2021, October 27). Steroid Injections. https://my.clevelandclinic.org/health/treatments/4812-steroid-injections
- Mayo Clinic. (2021, March 6). Cortisone shots. https://www.mayoclinic.org/tests-procedures/cortisone-shots/about/pac-20385216
Dr. Grant Fourie, a specialist in male hormones, is based in Cape Town, South Africa. He provides comprehensive treatments for conditions related to low testosterone, such as erectile dysfunction, fatigue, and mood changes. His methods include hormone replacement therapy and other modern treatment options.
Contact me via email or phone to book personal appointment in my clinic: The Village Square, Cape Town - South Africa



